Designer Drug Exposé: Introduction To Research Chemicals 🧪
These drugs are “not intended for human consumption…”

Nobody knows the exact number of psychoactive molecules that coexist in our world since most of them remain completely untested — and countless others have yet to be discovered.
Our database contains over 2300 psychoactive substances — over 70% of which have little to no formal research.
Today, artificial intelligence is being used to unlock new, undiscovered psychedelics at breakneck speed, and experimental psychonauts are racing to be the first to submit trip reports on new designer drugs.
The fact that even the tiniest molecular modifications can lead to dramatic shifts in cognition and perception is not only a fascinating topic to explore but also carries significant implications for our understanding of consciousness, mental health, and the potential therapeutic applications of these compounds.
Welcome to the mesmerizing world of designer drugs.
⚠️ Warning: All the designer drugs or "research chemicals" we explore with this series come with their fair share of risk. We know almost nothing about their toxicity, interactions with other drugs, or long-term side effects. Some of these substances are overtly toxic — always do your research before you embark 🚀
This post is for informational purposes only.
What is a "Designer" Drug?
A designer drug is any synthetic substance created with the intention to mimic the effects of known (usually illegal) psychoactive substances.
These new compounds circumvent existing drug laws by modifying the base chemical structure in such a way that it no longer fits the description of the illegal substance it's modeled after.
Traits of a designer drug:
🔬 Synthetic or semi-synthetic
🌀 Mimics the effects of established psychoactive drugs
⚙️ Structural modifications performed to avoid prohibition
🧪 Limited research or understanding of the nature of the drug
🚀 Niche interest among experimental psychonauts
🌍 Not included in any of the international drug control conventions
The term "designer drug" isn't perfect. There are many drugs that don't fit within this criteria that many people still consider designer drugs. For example, 2C-B is frequently referred to as a designer drug, yet it's been around since the 1970s and is officially recognized as a Schedule II drug by the UN Commission on Narcotic Drugs.
Other examples include etizolam, MXE, and GBL.
Another term some people use is "research chemicals." This term was coined in the 90s as a way for designer drug vendors to avoid "intent" clauses. Vendors sell these substances for research purposes — "not for human consumption."
Some also feel the designation of "designer drug" gives these substances an exclusive feel. “Research chemicals” does a better job of driving the point that we know nothing about the impacts these drugs have on the human body and psyche.
Government regulators like the DEA and UNODC have their own word. They call them "New Psychoactive Substances" or "NPS" for short. This is an even poorer term to describe the space these particular drugs fill — many of these substances aren't new.
For example, many chemicals developed by pharmaceutical companies in the 60s, 70s, and 80s that were abandoned or eventually banned by regulators are being rediscovered and sold as modern designer drugs. Etizolam, 2-Oxoquazepam, and BMS-906024 are all examples of this.
For every psychoactive drug listed on restricted substances lists, there are dozens of "designer drugs" with virtually indistinguishable effects.
As an example, let's look at LSD (lysergic acid diethylamide), one of the most popular psychedelics in modern history. LSD gets all the attention, but it's just one of over 20 closely related psychedelics in the lysergamide family.
AL-LAD, PRO-LAD, ETH-LAD, LSZ, 1P-LSD, and numerous others contain the same lysergic acid base structure, with slight variations on their functional groups that technically make them "not LSD" — even though their binding affinities and effect profiles are indistinguishable.
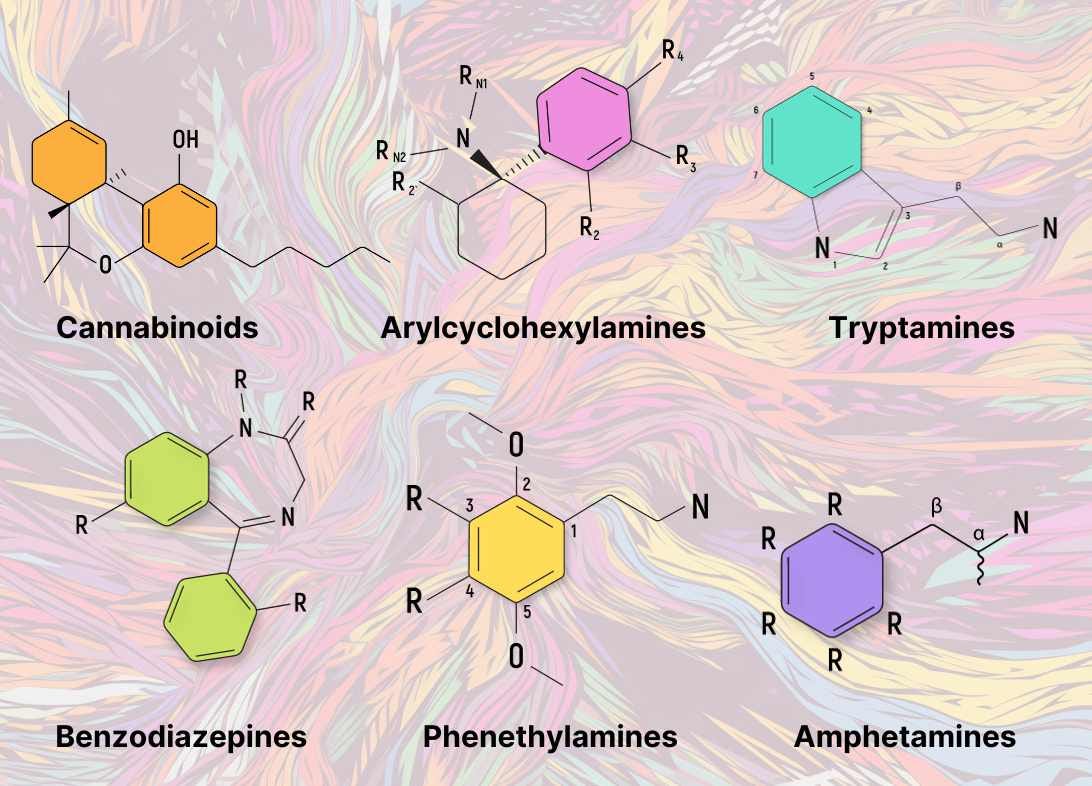
Designer drugs are available for every known psychoactive drug class — amphetamines, benzodiazepines, arylcyclohexylamines, cannabinoids, lysergamides, tryptamines, phenethylamines, piperazines, pyrrolidines, tropane alkaloids, oxazolidines, phenylmorpholines, opioids, and many more.
New designer drugs are created almost every day.
Are Designer Drugs Truly Legal?
Regulators and clandestine drug manufacturers have been playing a game of cat and mouse for decades.
A few years after a drug's creation, it's added to the restricted substances list. Chemists then modify the original molecule slightly to create a "new" drug to avoid this prohibition — rinse and repeat.
Some countries, including the United States, have tried to put an end to this by introducing laws that block the analogs of drugs included on the restricted substances list.
These laws work by imposing automatic bans on drugs that are sufficiently similar to illegal drugs.
In the US, the Federal Analogue Act was passed in 1986 as a response to the surging development of "designer drugs" — mostly fentanyl analogs at the time. The goal of the Federal Analogue Act was to make it possible to control designer drugs without having to ban each one individually — a process that takes years to complete.
These laws make sense on paper, but none of them have worked very well in practice.
The problem is that there's a lot of gray area around what actually qualifies a drug as "similar enough" to be illegal.
How similar does the drug have to be to be considered illegal? Is it the subjective effects that matter or the molecular structure? How is the average person supposed to know the exact chemical structure of a drug they bought?
These questions leave a lot of room for interpretation, which isn't conducive to a fair justice system. It's difficult for prosecutors to provide fair notice to the average person as to exactly which substances are illegal and which ones are not.
The problem falls on two key issues:
The sheer variability of psychoactive chemistry
The vague language regulators are forced to use to define "similarity"
The Analogue Act is easy to challenge in court, so most cases end up getting thrown out.
For example, in New York (2022), in a case involving the GHB designer drug, 1,4-butanediol, the judge ruled that the drug couldn't be considered an analog of GHB under federal law. The chemist called to the stand to testify stated that "... a student who stated on a college exam that GHB and 1,4-butanediol were similar in chemical structure would indeed fail such an exam."
The judge ruled that applying the Analogue Act would be unconstitutionally vague.
So, despite the introduction of the Analogue Act over 40 years ago, the designer drug market has only grown in size — reaching its zenith in the 2010s as a flurry of new drugs entered the clandestine market in a short period of time.
Even with the recent developments in the cannabis space — THCP, delta 8 THC, HHC, HHCP, THC-O, and dozens of others — there hasn't been much pushback against companies selling substances that could be technically viewed as illegal under the Federal Analogue Act.
To this day, most designer drugs are considered "illegal," but little is done to enforce these laws. Designer drugs are sold freely and openly on various online marketplaces and by street-level vendors.
Restricted Substances Lists:
Chemical Roulette: The Dangers of Designer Drugs
A core virtue of designer drugs is that they've never been formally tested. This is why many experts prefer the term "research chemicals" — referring to the fact that we know almost nothing about these chemicals, their safe upper limits, the long-term consequences, and potential interactions with other substances or supplements.
Most of the compounds considered "designer drugs" only have preliminary testing to determine their chemical structure, binding affinity on target receptors, and basic toxicity — but that's it.
Very few of these substances have been properly tested for safety in humans — of the ones that have, most have shown unfavorable results, which is why they never made it to market in the first place.
This is the case with many of the designer benzodiazepines, amphetamines, and arylcyclohexylamines — first developed by pharmaceutical companies, sometimes dating back as far as the 1950s.
For a drug to be approved for use in humans, millions of dollars must first be spent testing through rigorous phase I, II, and III clinical trials. When drugs produce too many side effects in clinical testing, they're often abandoned.
This is the reason why most designer drugs have not and likely will not ever be formally tested. Companies will only fork out millions of dollars to properly explore the long-term safety and efficacy of a substance they can patent and profit from.
Here are some of the inherent risks that come with all forms of designer drugs:
1. Dosing Variability
Some compounds are active in sub-milligram doses (<1 mg), while others require several grams (>1000 mg). This is a massive variability in dosing.
Taking several milligrams of a potent drug like fentanyl or triazolam could easily lead to an overdose.
With designer drugs, the potency is often unknown. Experts like Alexander Shulgin approached them very cautiously by first taking just a few micrograms, then a milligram, then 2, and so on until he discovered the threshold dose.
This is not the case with the general designer drug community, who tend to just "eyeball" their doses. There are many cases where people have died from simple ignorance like this.
2. Unscrupulous Vendors & Adulteration
The designer drug market has always been a Wild West. There are plenty of cases where vendors list something popular, like 2C-B or MDMA, but instead ship something cheaper to manufacture.
Cheaper usually means more potent. For example, opioids are often cut with potent fentanyl analogs and fillers. The main problem with this (aside from being sold something you didn't intend to buy) is that highly potent drugs like fentanyl are much more dangerous.
It's common for careless drug dealers to mistakenly add too much of the drug. When users prepare their usual dose, they're hit with a dose many times higher than anticipated — often resulting in injury or death.
This problem is also common in the lysergamide space, with some vendors selling NBOMes in place of LSD. The effects of this drug are similar, but NBOMes take much longer to kick in and have a very serious potential for overdose.
Once people become impatient that their acid isn't working, they double down with another dose. An hour or two later, both doses kick in. There have been a number of deaths reported from NBOMe consumption because of this exact issue.
This is why it's critical to be skeptical about drugs ordered over the internet. Buy a cheap reagent test kit and test a sample of everything BEFORE you take it.
3. Impure Chemicals
Synthesizing pure chemicals is difficult, and many of the manufacturers making these drugs lack sufficient skill and experience to produce them safely. These products often contain harmful byproducts that should have been filtered out and removed from the final product.
A good example of this involved a drug called MPPP. This drug was developed as an alternative to Meperidine (pethidine). If MPPP isn't synthesized by an expert chemist, an impurity called MPTP would often wind up in the final product.
MPTP is now well known to cause brain damage — often after a single use. People who used this drug wound up with a syndrome indistinguishable from late-stage Parkinson's disease.
4. Unknown Toxicity
Even if used at the right dose, there's always a risk that a new chemical that just entered the market could pose its own inherent dangers — regardless of getting the dose right or not.
The only way we know which drugs are dangerous is because someone, somewhere, either died or nearly died from taking them. Often, single cases aren't significant enough to make the news, so it can sometimes take multiple deaths before word gets out that a new designer drug is dangerous.
Harm Reduction Tips for Designer Drug Exploration
🧪 Always test a sample of your substance using reagent test kits
📚 Do your research — learn about dosing, side effects, and interactions with other substances. Use multiple sources to gather your information.
👀 Don't eyeball your dose — use a scale
🔬 Start low and go slow — always take less than you think you need for the first dose. You can always take more, but you can't take less.
🥣 Avoid mixing substances
🐺 Don't trip alone — always have a trusted tripsitter
🎃 Never attempt to trick or persuade someone into using a substance they don't want to take
🚗 Don't swim, drive, or operate machinery while taking intoxicating substances
💊 Talk to your doctor first if you're taking ANY prescription medications or have a diagnosed medical condition
The Evolution of Designer Drugs
Designer drugs have been around for nearly 100 years — but the landscape has changed dramatically in that time — and with the introduction of AI-fueled drug discovery, it's going to change a lot more within the next few decades.
1925–1960
A reasonable starting point for outlining the history of designer drugs is 1925. This was the year the 1925 Opium Convention officially passed. This convention set in motion a banning of the opioids morphine and diamorphine (heroin). Morphine was maintained in medical practice, but heroin was outlawed entirely.
In 1930, the first analog act was passed that restricted the sale of morphine esters, including both oxycodone and hydromorphone. This was the first law addressing the analogs of known restricted substances.
Alcohol was also banned for 13 years during this era. The prohibition was introduced by the 18th Amendment to the US Constitution and remained in place from 1920 until 1933. Despite the ban, demand for alcohol remained high. Many turned to underground illegal bars, while others turned to the nearest "designer alcohol" — diethyl-ether.
1960–1980
The 60s saw a surge in psychoactive drug use. This was the time when LSD was unleashed onto the world along with a variety of other synthetic psychedelics like DOM and ALD-52.
This was also the period when pharmaceutical companies were hard at work developing new amphetamine-based stimulants, benzodiazepines, and opioids. Several of these drugs achieved blockbuster status, while the majority were left unexplored or abandoned.
Many of the compounds discovered during this era were revived decades later as designer drugs.
1980-1990
The term "designer drug" was coined in the 80s. At the time, it mainly referred to the influx of opioid drugs based around fentanyl and meperidine dealers were using to adulterate heroin.
In 1984, the DEA was granted the power to emergency ban chemicals for one and a half years under the Comprehensive Crime Control Act of 1984. At the end of the temporary ban, the DEA had to provide a convincing case to establish a permanent ban.
This power was used for the first time in 1985 for MDMA. It's been used many times since for drugs, including 2C-B, AMT, and BZP.
The Federal Analogue Act, as we know it today, was introduced in 1986.
1990–2010
Alexander and Anne Shulgin published their seminal book on phenethylamine analogs, PiHKAL, in 1991. Half the book provided detailed recipes for synthesizing the many novel psychedelic substances Alexander created himself in his lab. The other half detailed the love story between the two authors. T
his book sparked a ton of interest in designer drugs and led to the Shulgin's (legal) home lab being raided and shut down by the DEA.
The late '90s and early '00s saw a dramatic uptick in designer drug sales. Significant connectivity through the World Wide Web led to a surge of online shops selling "legal highs."
The term "research chemical" first appeared around this time as online drug vendors tried to legitimize the drugs they were selling. The idea is that by selling them as "research chemicals" and "not for human consumption," they could avoid the intent clause included in the Analogue Act. Basically, vendors could claim they never intended for their products to be consumed — merely studied.
The first synthetic cannabis products started hitting the shelves of headshops around the United States in 2008. The first two compounds to appear on the DEA's radar were JWH-018 and CP 47,497. They were sold as "incense, not for human consumption."
By 2010, there were dozens of these compounds on the market. Most of the time, they were combined in various blends and sprayed onto the dried leaf material of plants like damiana, mugwort, or mullein.
The drugs known colloquially today as "bath salts" also made their debut in the late '00s with the introduction of mephedrone and MDPV in headshops and online smart shops.
2010–Present
The 2010s saw a continued expansion of the designer drug development. The vast majority of designer benzodiazepines, arylcyclohexylamines, as well as a multitude of novel drug families like benzofurans, diarylethylamines, tropanes, and methaqualones have appeared on the designer drug market since 2010.
This period also marked a dramatic uptick in the "alt cannabinoid" market. Unlike the "not for human consumption" synthetic cannabinoid craze of the previous decade, this go-round involved exploiting a loophole in the 2018 Farm Bill. The Farm Bill is reviewed and updated every 4-years. With the most recent update, the bill made any Cannabis sativa plant that produced less than 0.3% delta-9 THC legal.
These plants are deemed "hemp," while anything that exceeds the 0.3% threshold is considered "marijuana." This loophole allowed manufacturers to convert CBD (which is abundant in hemp) into delta-8 THC, delta-10 THC, HHC, THCV, THCP, and various others.
All of these cannabinoids work the same way as delta-9 THC found in marijuana — but because the Schedule I listing specifically lists only the delta-9 isomer, these other analogs are all considered legal.
Regulators appear to be having a much tougher time banning substances than they used to.
For example, the DEA's attempt at banning five tryptamine psychedelics in 2022 was shot down during the public comment period. This comment period is a mandatory step when moving to ban substances. The same thing happened in 2016 when the DEA tried to ban kratom —an important plant-based stimulant and alternative to synthetic opioids.
The DEA did have a few successes, however — for example, Flakka (alpha-PVP) and 9 other cathinones in 2014, U-47700 in 2016 and six more synthetic cathinones and the benzodiazepine drug etizolam in 2022.
Of course, the problem is that banning a substance never makes it go away — not entirely. New drugs are being discovered at such a breakneck speed that eliminating psychoactive drugs from the market is like trying to catch smoke.
Where Do We Go From Here?
The history of designer drugs continues to evolve, with new substances and analogs emerging almost weekly. There's now a vast selection of designer drugs available online — and it's only going to expand.
The introduction of AI in recent years has significantly increased the rate of drug development. In 2020, a team of researchers at the Massachusetts Institute of Technology trained an AI to discover a new antibiotic by first teaching it about 2,500 known antibiotics, then submitting 6,000 novel compounds and asking the computer to pick out the ones that likely had the greatest efficacy against a drug-resistant strain of E. coli. In a matter of minutes, the AI had its choice — this drug is now called halicin, and it's now well on its way to being a revolutionary new medicine.
AI is already being used to speed up the discovery of new psychedelics, but most of this work is taking place behind closed doors in the basement of psychedelic startups. Companies like MagicMed Industries (recently acquired by Enveric Biosciences) are using AI to rapidly discover new psychedelic molecules they can patent and release onto the world.
So far, they've built up an impressive portfolio (called their "Psybrary"), which includes 15 individual patent families and several hundred new psychoactive molecules.
Even without AI, there's never a shortage of experimental humans looking to try drugs nobody else has before. Amateur psychonauts and chemists are teaming up to synthesize or otherwise source these novel psychoactives and post their trip reports online.
It's become a badge of honor for some to post the very first trip report on subreddits like /r/drugs, /r/researchchemicals, /r/dissociatives, /r/stims/ or any of the other designer drug communities.
Regulators at both the municipal and federal levels have been pushing for the removal of drugs with very low-risk profiles. Drugs like marijuana, LSD, magic mushrooms, and mescaline all fall into this group — a fact that's been established by the countless individuals who have taken these substances.
The same can't be said for random synthetic cannabinoids, mescaline-like analogs, or NBOMe-based LSD alternatives.
In this ever-evolving landscape of designer drugs, the future remains both promising and uncertain. The vast array of new substances available online continues to grow, driven by advances in technology, including the remarkable capabilities of AI.
As with any psychoactive substance, it's important to remember that there's no such thing as a good or bad molecule; it's our relationship to them and the way we use them that can be good or bad.
We’ll be releasing the next four parts of this series over the next few weeks.
We’ll take a deep dive into specific families of drugs and explore the landscape of the many designer drugs available for each one: