Rewiring the Mind: How Psychedelics Offer Hope for Alzheimer’s Disease
A new wave of research suggests psychedelics may offer a novel approach to managing Alzheimer's disease by promoting neuroplasticity, reducing brain inflammation, and improving emotional wellbeing.
Forgotten keys, the names of distant relatives, or even the reason you walked into a room — these memory lapses are common experiences. But at what point do these everyday forgetfulness signs indicate something more serious? And what options are available when they do?
When confronting a neurodegenerative condition like Alzheimer’s disease, these questions are just the tip of the iceberg.
Alzheimer’s is a debilitating neurological condition that accounts for a majority of dementia cases. While great strides have been made in our fundamental understanding of Alzheimer’s and its progression, treatment options are still limited, with incredibly few FDA-approved treatments available to the public today.
Several medications do exist to manage the symptoms of Alzheimer’s disease, but this is no easy task, and there is heavy debate on whether the side effects of these treatments are even worth it.
In recent years, evidence has been mounting regarding the potential for psychedelics to enhance neuroplasticity — the brain's ability to form new connections.
Over time, it’s becoming apparent that the intersection of psychedelic research and Alzheimer’s might offer long unanswered questions about the aging brain.
But the question still stands — are psychedelics truly a viable solution for treating Alzheimer’s disease?
The Discovery of Alzheimer’s
In 1901, a physician by the name of Alois Alzheimer came across a patient with an unusual case. The patient, Auguste, had been experiencing eight months of changes to her personality and severe memory impairment.
Auguste frequently found herself lost in familiar situations and fearful of people she knew well. Rife with confusion and fits of jealousy and occasionally imagining that someone wanted to kill her, her husband brought her in to be examined at a psychiatric institution in Frankfurt.
Auguste’s case was of particular interest to Dr. Alzheimer, who had never seen symptoms quite like hers before. He decided to follow her case closely to track her mysterious condition.
In his initial interviews with Auguste, Dr. Alzheimer noted that she would speak clearly and articulate well but would often stop midway through her sentence as if she had become lost.
Over time, her demeanor went from generally anxious, confused, and disoriented to distant, unintelligible, and aggressively reactive. Eventually, Auguste stopped talking altogether and in her final years, became completely apathetic and recluded to her bed.
Perhaps the most tragic and succinct summary of the changes Auguste experienced is from her own remark on her state, “I have, so to say, lost myself.”
Dr. Alzheimer was not convinced that Auguste's symptoms were psychiatric in nature. When she passed away, Dr. Alzheimer examined sections of her brain under a microscope and found widespread atrophy — a massive loss of cells throughout the brain.
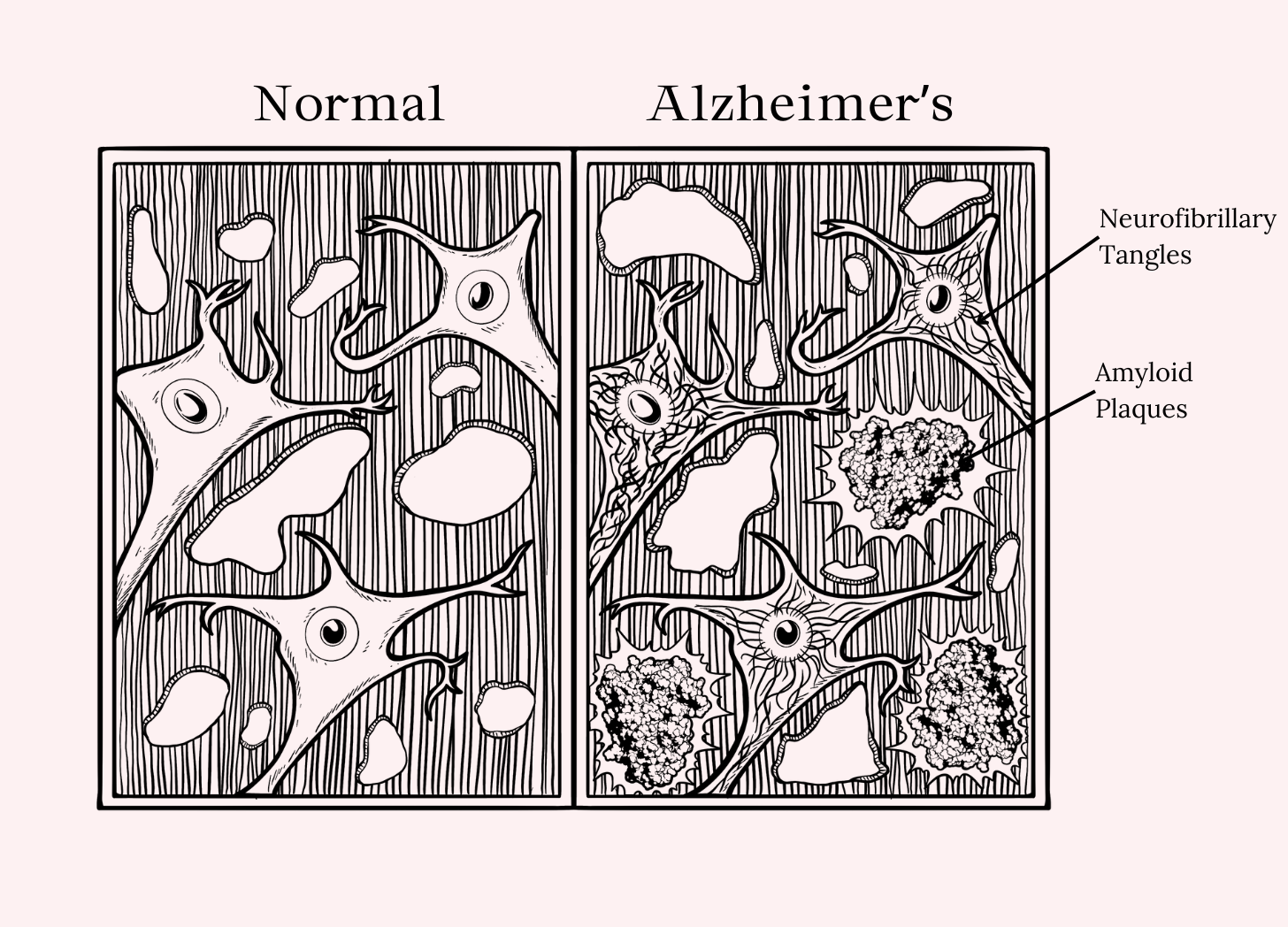
He also discovered thick fibrils called neurofibrillary tangles within the neurons and an unidentified substance, now known as amyloid plaques.
In this discovery, Dr. Alzheimer found what would become known as two of the defining features of Alzheimer’s disease today and set the stage for understanding this neuropathological disease.
What Causes Alzheimer's Disease?
Before we get into the weeds about how researchers believe certain psychedelic substances can be used to counteract the devastating effects of Alzheimer's disease, it's important to understand what, exactly, is happening in the Alzheimer's brain:
Alzheimer’s disease is characterized by two key pathological features:
A formation of neurofibrillary tangles made up of dysfunctional TAU proteins.
Plaques consisting of a sticky compound called amyloid-beta that forms around the neurons.
Over time, TAU proteins and amyloid-beta plaques cause damage to the neurons by choking them out and disrupting their ability to function — ultimately leading to widespread neuronal death and inflammation.
As our neurons die, we experience lapses in memory and cognitive decline (confusion, disorientation, mood changes, and difficulty communicating with others).
1. TAU Protein Tangles
TAU proteins are normal components of a healthy brain. They're used to stabilize a group of structures called microtubules that help transport nutrients within the cell.
For reasons not well understood, Alzheimer's disease sufferers have a problem regulating these TAU proteins. They become hyperphosphorylated, which causes them to misfold and form thick tangles that not only don't function as intended but also actively disrupt the neuron's ability to transport nutrients.
This eventually causes the neuron to die.
2. Amyloid-Beta Plaques
Amyloid-beta is another completely normal byproduct of healthy neurons. It forms when another compound called amyloid precursor protein (APP) breaks down.
Normally, this protein is cleared from the neurons by the glymphatic system before it can cause any damage. However, patients with Alzheimer's disease are unable to effectively remove this sticky substance. The exact reasons for this remains unknown. As amyloid-beta accumulates in the brain, it begins to form a thick plaque on the outside of neurons, disrupting communication between them and further contributing to neuronal damage and inflammation.
3. Inflammation
Inflammation is a secondary effect of Alzheimer's disease. As TAU proteins and amyloid-beta wreak havoc on the neurons, the dying cells release proinflammatory cytokines that signal widespread inflammation throughout the brain.
This inflammation further worsens neuronal damage and can cause harm to other unaffected regions of the brain.
Chronic (long-term) neuroinflammation has been linked to difficulty sleeping, anxiety, and depression — just to name a few.
Pitfalls in Current Alzheimer’s Disease Therapy
There are currently only two FDA-approved treatments for Alzheimer’s that target the underlying mechanisms of the disease.
The medications, aducanumab, and lecanemab, were only approved in 2021 and 2023, respectively, and are designed to target and reduce the presence of amyloid-beta plaques.
There's a great deal of controversy around these medications, as it is still uncertain whether the reduction of amyloid plaques can actually translate into meaningful clinical benefits (evidence is mixed on this matter, with some finding marginal improvements and others showing no functional improvement whatsoever).
High costs and the risk of serious side effects such as brain swelling and bleeding further add to the debate about whether the benefits of these medications outweigh the risks.
Ultimately, the efficacy of these treatments remains questionable, leaving a significant gap in effective Alzheimer’s therapies.
Can Psychedelics Slow the Progression of Alzheimer’s Disease?
There are thousands of known chemicals, natural or synthetic, that could be considered “psychedelic.”
Only a tiny fraction of these compounds have been explored as a potential treatment for brain disorders like Alzheimer's Disease.
For the purposes of this discussion, we're specifically talking about "classical psychedelics" — which include tryptamines like LSD (lysergic acid diethylamide), magic mushrooms (psilocin & psilocybin), and DMT (dimethyltryptamine), and certain phenethylamines like mescaline or DOI.
These psychedelics all work through a similar mechanism of action — they mimic the neurotransmitter serotonin.
There are 15 different types of serotonin receptors in the brain — each one involved with regulating different processes. Psychedelics can bind to various serotonin receptors but are especially active on a particular subtype called 5-HT2A. The activation of this serotonin receptor subtype is critical for the psychedelic experience to take place.
What makes this receptor even more interesting is its apparent role in regulating neuroplasticity — which is the ability of the neurons to adapt and reorganize — restructuring themselves and forming new connections with neighboring neurons.
The ability to support neuroplasticity is considered the key mechanism for the therapeutic potential of psychedelics in the treatment of neurodegenerative disorders like Alzheimer's disease as well as depression and PTSD.
Before we get into the specifics of how researchers are testing the use of psychedelics for Alzheimer's disease, I have to issue a disclaimer:
As of right now, there is no conclusive evidence that psychedelics can directly treat the disease in the same way that amyloid-targeting drugs like aducanumab or lecanemab do. The research we're going to explore below is mostly theoretical and addresses more of the underlying mechanisms involved with the disease.
With that said, there are some very promising preclinical studies and early-stage research that suggest psychedelics like LSD, psilocybin, and DMT may provide a novel approach to fighting or even preventing the development of Alzheimer's disease.
Here are the highlights:
Keep reading with a 7-day free trial
Subscribe to Tripsitter to keep reading this post and get 7 days of free access to the full post archives.