High Hopes: Can Psychedelics Mark A New Era In Pain Management?
In the quest for pain relief, the next breakthrough might just be psychedelic.
Pain is notoriously difficult to treat and stands as a leading cause of disability. Given that conventional pain medications fall short of providing long-term relief, it's no wonder people have turned to the wildly innovative field of psychedelic medicine to search for alternatives.
Though unconventional, this choice appears to hold promise. There have been increasing accounts of people self-administering psychedelics to manage pain, and researchers have shifted focus to figure out how it works.
So far, studies suggest psychedelics target both the physiological causes of pain as well as psychological ones. For example, some studies have found psychedelics alter the meaning we assign to pain, which can profoundly reduce its influence.
Here, we’ll dive into the latest findings on the effectiveness of using both micro- and macrodoses, explore a range of pain conditions that psychedelics may offer relief for, and see how they compare to conventional pain meds.
We’ll also explore insights from Mauro Cavarra — a pioneering researcher in the field of psychedelics and pain — and shed light on how these substances may soon revolutionize our approach to pain management.
Can Psychedelics be Used to Treat Pain?
Recent evidence suggests that classic psychedelics such as LSD (lysergic acid diethylamide) and psilocybin (magic mushrooms) could serve as a potential treatment for several types of chronic pain.
In some cases, individuals report psychedelics outperform their conventional medications, which include nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and antidepressants — especially with long-term use.
So far, psychedelics have been studied for treating the following conditions:
Cluster headaches
Phantom limb pain
Fibromyalgia
Arthritis
Migraines
Tension-type headaches
Sciatica
For all the conditions above except for sciatica, there’s been evidence from survey data and proof of concept studies that psychedelics have at least some degree of effectiveness.
Currently, the research focuses mainly on chronic pain conditions, and it's uncertain whether psychedelics are effective for acute (short-term) pain or not.
Disclaimer: While results are promising, it should be noted that this research is still in the early stages. It’s too soon to make any definitive claims.
Psychedelics & Pain Tolerance: Surprising Findings From LSD Research
A study from 2021 examined the effects of low-dose LSD (20 μg) to see what impact the substance had on one's ability to tolerate different levels of pain.
The study found a clear decrease in subjective levels of experienced pain and unpleasantness.
This study used the cold water test — which is a classic measure to determine changes in pain tolerance over time. Participants dip their hand in ice water (3ºC) while scientists use machines to measure their physiological reaction to the discomfort.
The increase in pain tolerance that participants given low-dose LSD experienced is comparable to that of opioids when undergoing the same cold water test.
The results suggest that even without mind-altering effects, at low doses, psychedelics can be used as a form of pain management.
Micro vs. Macro: Sizing Up Psychedelic Doses
A survey of 250 chronic pain participants found that while full psychedelic doses are less commonly used for pain management, they appear to be more effective than microdoses. The same survey also noted that full-dose psychedelics were more effective than conventional pain medications — including opioids and cannabis.
This doesn’t mean that microdoses are ineffective — the survey still noted marked improvements in those who took microdoses to ease pain — just that the effects of microdoses are not as potent and are more susceptible to expectation bias.
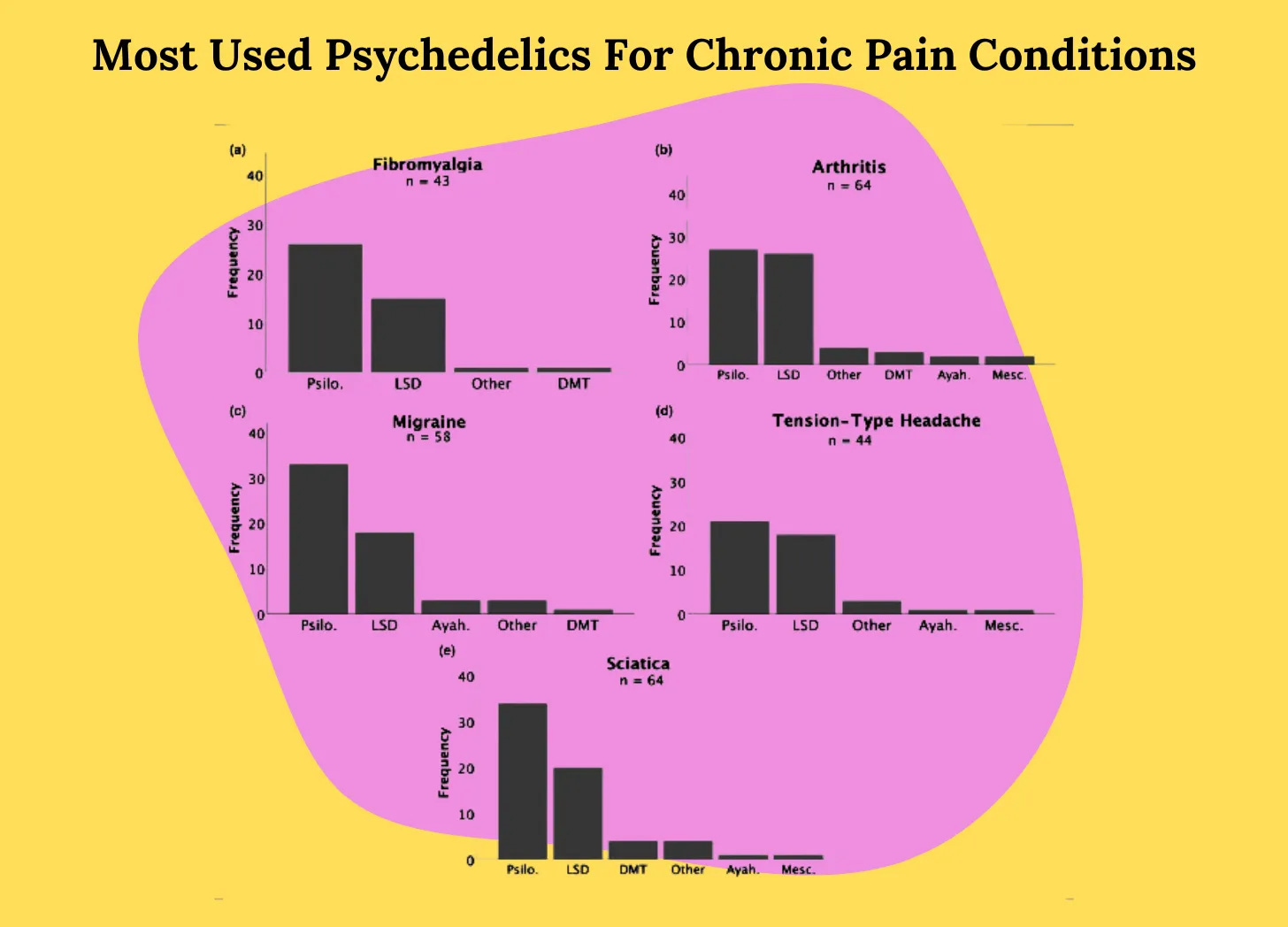
Out of this group, psilocybin was the most common psychedelic used, with LSD coming in second.
A microdose, in this case, was defined as one-tenth to one-twentieth of a dose, while a full dose entailed significant alterations in consciousness states.
Psychedelics & Chronic (Long-Term) Pain
As of right now, survey data supports that full doses are at least partially effective when compared with conventional medications for chronic pain conditions, including migraines, fibromyalgia, arthritis, and tension headaches.
Case studies and anecdotal reports have shown that psychedelics can be effective for phantom limb pain when combined with mirror visual feedback.
Mirror visual feedback, also known as mirror therapy, is a therapeutic technique that uses a mirror to create a reflective illusion of an affected limb to trick the brain into thinking movement has occurred without pain or impairment.
Lastly, a proof of concept study for cluster headaches and microdoses of psilocybin found mixed results, with some participants experiencing complete remission — but not others.
Understanding Pain: Beyond the Physical Sensation
Pain is a protective mechanism. You can think of the classic example of a hand on a hot stove and pain serving as your body's way of warning you of physical harm, whether internal or external.
Nociceptors are the specialized receptors throughout the body that warn us of potential harm, such as extreme temperatures, intense pressure, or inflammation. However, signaling from these receptors is not a direct measure of pain.
A lack of direct measures makes pain difficult to treat. The problem is that the physiological cause of pain may be minor, yet the pain experienced is great — and vice versa.
What’s known about pain is based purely on subjective experience.
The International Association for the Study of Pain (IASP) emphasizes that pain is a personal and learned phenomenon and that a person's individual report of pain should be respected.
Psychedelics vs. Traditional Pain Meds
Treating pain is as much a psychological battle as it is a pharmacological one, as many chronic pain patients simultaneously struggle with depression.
As of 2024, the most common pain medications include:
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Opioids
Anti-seizure medications
Antidepressants
Generally, these medications work by treating enzymes or chemical messengers involved with pain and/or inflammation. Antidepressants such as serotonin-norepinephrine reuptake inhibitors (SNRI) serve a dual purpose of treating chemical processes that cause pain while also addressing the negative impact pain has on mood.
The issues surrounding current pain medications include a long list of side effects as well as questions about long-term efficacy. Remarkably, despite opioids being the most commonly prescribed painkiller, according to CDC guidelines, there are no studies reporting long-term (>1 year) benefits of opioids for chronic pain.
On the other hand, psychological treatments such as cognitive-behavioral therapy (CBT) and mindfulness-based interventions are consistently associated with better outcomes in reducing pain intensity and increasing quality of life than pharmacological treatments alone.
The advantage of psychedelics is that they provide a means to treat pain holistically (with both physiological and psychological components) while circumventing the side effects of conventional pain meds.
There are several theories as to how psychedelics treat pain. The most prominent suggests a modulation of 4 key factors:
Dendritic plasticity
Stress Hormones
Serotonin (5HT2A) Receptors
Immune System

Chronic pain can cause alterations in the nervous system, which psychedelics can potentially remedy by reorganizing the brain networks that may have been disrupted. Psychedelics can also have anti-inflammatory effects, which are especially useful in treating chronic and functional pain disorders like migraine and fibromyalgia.
Future research is still needed to support these proposed theories.

How Psychedelics Can Redefine The Meaning We Attach to Pain
The way we perceive pain is intertwined with the meaning we assign to it — and psychedelics offer a fascinating pathway to reshape our perceptions.
For instance, a group of participants in a study, unaware they're about to feel a cold metal bar against their skin, are told it's “very hot.” Surprisingly, the participants told this false information experience the sensation as being more painful. This difference in perception illustrates how our interpretation of pain can alter its intensity.
Similarly, consider a patient grappling with back pain from a herniated disc. If they have an understanding of the root cause of their discomfort, such as a compressed nerve, they likely experience less pain.
So, how can psychedelics help with this?
Mauro Cavarra, psychotherapist and PhD candidate at Maastricht University, is a leading researcher in the field of psychedelics and pain. From his research, Cavarra shares a case study where a participant transforms their relationship with pain by imbuing it with new meaning after an experience with psychedelics.
This case study follows a patient suffering from fibromyalgia before and after attending a psychedelic retreat center.
Over several months, the patient noted a dramatic transformation not only in the level of pain they experienced — but also in the way they interpreted the "meaning" of their pain.
Before the retreat, they described the pain as something external, enduring, and over which they had no control. After the retreat, they interpreted the pain as a sign that they needed to change some aspect of their life.
Consequently, over six months, this participant made significant changes in their life — changing jobs, connecting with different social circles, adopting a more proactive attitude towards their health, and adjusting the relational dynamics they believed to be contributing to their pain.
As Cavarra elucidates, "When people give meaning to their pain, the pain becomes more manageable and reduces its intensity."
This case study illuminates a new avenue through which psychedelics can offer relief from pain and underscores the importance of guidance in pain management.
Psychedelics, in conjunction with psychotherapy, offers an innovative approach to pain management that addresses both the physiological causes of pain, and the psychological and emotional components that perpetuate and intensify it.
More Mauro Cavarra Research on Psychedelics & Pain:
Potential analgesic effects of psychedelics on select chronic pain conditions: A survey study (2024)
Psychedelic-Assisted Psychotherapy: A Systematic Review of Associated Psychological Interventions (2022)
Next Steps for Psychedelic Pain Research
There are still big questions to be answered in terms of the effectiveness of psychedelics for treating pain.
The findings so far emphasize the need for clinical trials as a necessary next step to provide a more scrutinizing look.
With more controlled studies, we can answer pressing questions such as:
Which psychedelics are most effective?
How long do the painkilling effects of psychedelics last?
What types of pain are psychedelics most effective at treating?
What are the long-term implications of using psychedelics to treat pain?
Already, psychedelics are offering us a completely new approach to managing pain. The idea that we can change the meaning we assign to our pain to reduce its influence and severity marks a profound gap in our current arsenal of treatment options.
Further Reading
Can Psilocybin Treat Cluster Headaches? (Tripsitter)
Adapting Psychedelic Medicine for Headache and Chronic Pain Disorders
Can Psychedelic Drugs Treat Physical Pain? (Scientific American)
Ketamine & Fibromyalgia Pain (Tripsitter)
Ketamine For Pain Management (Tripsitter)
Enjoying the Trip? 🍄
Don’t Journey Alone! Tripsitter was built by a community of psychedelic advocates — but it’s people like you that allow us to thrive.