Designer Drug Exposé: Sedative Hypnotics & Opioids
While psychedelics expand consciousness, designer sedatives and opioids aim to suppress it — creating a growing underground market for chemical oblivion.

The line between medicine and mayhem has never been thinner than in today's designer sedative market.
Unlike psychedelics that alter perception or expand consciousness, these compounds suppress consciousness. They're designed to induce chemical oblivion.
Could the rise of designer downers signify a deeper societal shift — where increasing numbers seek to escape all forms of conscious thought and emotional pain rather than process it?
Whatever the underlying cause, these substances represent some of the most dangerous and addictive compounds in the underground drug market. Many of the new drugs available today are thousands of times more potent than their legal counterparts.
The legitimate sedative market is enormous — over 100 million benzodiazepine prescriptions and 125 million opiate prescriptions are written annually in the US alone. The US markets for these drugs is currently valued at $2.5 billion and $14.5 billion, respectively.
The illicit side of this market is equally immense — estimated to exceed $1.5 billion for illicit benzodiazepines and a massive $10-12 billion for illicit opioids in the US alone.
Strict regulations, high costs, and the notoriously addictive nature of sedative and analgesic drugs in general, have created the perfect conditions for a thriving designer drug market.
Designer sedatives and opioids replicate the effects of established pharmaceuticals while skirting legal restrictions. The results are often unpredictable and dangerous — synthetic opioids like fentanyl analogs are now responsible for the majority of drug overdose deaths in the United States (around 70%) — and newer, even more powerful compounds are released every couple of years.
Some experts believe that with the introduction of open-source AI chemistry models, this arms race is only going to get worse — accelerating the development of untested, hyper-potent molecules that can be synthesized with minimal resources and devastating effect.
In this article, we'll explore the major classes of designer sedatives and opioids:
Benzodiazepines (DBZDs) — Novel variants of prescription anti-anxiety and sleep medications.
Methaqualones — Modern versions of the notorious 1970s "Quaaludes."
Opioids — Fentanyl analogs and other new synthetic classes.
Morphinans — A diverse group with both sedative and dissociative effects.
GHB Analogs — Legal and quasi-legal alternatives to traditional depressants and alcohol.
Volatile Anesthetics — Historical surgical drugs repurposed for recreational sedation.
Chemical Oblivion: The Neurochemistry of Sedation
Before diving deeper into the designer sedative landscape, it's important to understand what these substances actually do — and how they manipulate consciousness. There are two relevant actions here.
Sedatives — these compounds reduce anxiety and promote relaxation (sort of like dimming the lights). They have a calming effect but don't necessarily induce sleep at normal doses.
Hypnotics — these substances are specifically designed to produce blackout. While they also have sedative properties, their primary purpose is a full shutdown of consciousness.
Most of these drugs work by boosting GABA, the brain’s primary inhibitory neurotransmitter. GABA slows electrical activity between neurons — leading to relaxation, disengagement, and in higher doses, deep sedation or unconsciousness.
Because GABA governs mood, attention, and arousal, altering this system doesn't just slow the brain — it changes how reality feels.
This is why GABAergic drugs (including, but not limited to alcohol) can make you feel drunk. Speech slows. Balance falters. Emotions feel exaggerated or numbed. Internal dialogue goes quiet. Thought loops dissolve into stillness or apathy. The brain's usual filters loosen — making some users feel open, euphoric, or uninhibited, while others feel foggy, detached, or lost in slow motion.
These compounds don't just dull the senses — they distort the way you process the world around you.
Different substances tap into GABA in unique ways:
Benzodiazepines increase the frequency of GABA-A receptor activity
Barbiturates prolong channel opening (dangerous and rarely used today)
Z-drugs target selective GABA receptor subtypes
GHB hits both GABA-B and dedicated GHB receptors
Alcohol enhances GABA along with other neurotransmitter systems
Opioids, though sedating, work differently — they bypass GABA entirely to suppress other brain regions (via opiate receptors) that are responsible for pain, alertness, and wakefulness.
Without further ado, let us descend into the shadowy world of sedatives and hypnotic drug classes:
Designer Benzodiazepines (DBZDs)
Designer benzos are a booming subclass of synthetic depressants modeled after pharmaceutical benzodiazepines — the so-called “chill pills” used to treat anxiety, insomnia, seizures, PTSD, and more.
All benzodiazepines share a common core structure: a benzene ring fused to a diazepine ring. They work by amplifying GABA, which leads to a deep sense of calm, sedation, and muscle relaxation.
At low doses, benzos ease anxiety. At high doses, they can induce blackouts, slurred speech, and alcohol-like intoxication. When mixed with other depressants (like opioids, alcohol, or GHB), the risk of overdose increases dramatically.
There are hundreds of benzodiazepine-like compounds — most developed during the pharmaceutical boom that took place between the 1960s and 1980s. Many were shelved before approval, but in today’s gray market, they’ve found new life as designer benzodiazepines (DBZDs).
These compounds appeal to users for two main reasons:
Cost & access — they’re cheaper and easier to obtain than prescription benzos
Potency — some DBZDs are stronger or longer-lasting than their pharmaceutical counterparts
Unlike approved drugs like Xanax, Valium, or Klonopin, most DBZDs have never passed clinical trials — meaning their safety profiles are poorly understood. A few, like etizolam and phenazepam, have been approved in limited countries and blur the line between pharmaceutical and research chemical.
According to the EMCDDA, these five compounds make up ~80% of all DBZD tablets found in Europe since 2005:
Etizolam — Short-acting, often mistaken for Xanax
Diclazepam — Diazepam analog with long half-life
Flubromazolan — Extremely potent, high overdose risk
Phenazepam — Long-lasting; approved in Russia
Pyrazolam — Mild, functional, often used for anxiety
But that’s just the surface. Dozens more DBZDs are active in the wild — many only loosely tested, yet readily available online.
Benzo Subclasses: Structure Over Function
While all benzodiazepines work by enhancing the effects of GABA they don’t all behave the same way. In fact, there are many distinct classes of benzos, each containing dozens (sometimes hundreds) of unique molecules.
Functionally, nearly all benzos induce calm, sedation, muscle relaxation, and anxiety relief. What sets them apart is:
Onset — how quickly they take effect
Duration — how long they last (short, intermediate, or long-acting)
Potency — how strong they are at a given dose
The most common way to group benzos is by their onset and duration of effects:
Short-acting DZBDs similar to Xanax (alprazolam) or Halcion (triazolam) include adinazolam, bentazepam, bretazenil, flunitrazolam, metizolam, oxazolam, and premazepam.
Intermediate-acting DZBDs similar to Klonopin (clonazepam) or Ativan (lorazepam) includes clonazolam, demoxepam, flubromzolam, nitemazepam, and others.
Long-acting DZBDs similar to Librium (chlordiazepoxide) and Valium (diazepam) include flubromazepam, fosazepam, gidazepam and phenazepam.
Beyond duration, there's a stunning diversity of molecular architecture in the benzodiazepine family. Structural differences influence their effects, metabolism, potency, and popularity in the designer drug market.
There are currently 14 benzodiazepine subgroups (a few are merged below):
1,4-Benzodiazepines — The oldest and most widely prescribed class. Includes Valium, Librium, Klonopin. Typically long-lasting with strong sedative properties.
1,5-Benzodiazepines — Structurally similar to 1,4-BZDs but with nitrogen in a different position. Slightly less sedating — often preferred for daytime use. Some members show unusual effects like antifungal or anti-inflammatory activity.
2,3-Benzodiazepines (GYKIs) — Atypical benzos with little to no GABA activity. Instead, they modulate AMPA receptors, with potential applications in neurodegenerative diseases — not common in the recreational market.
Triazolobenzodiazepines (TBZDs) — Among the strongest benzos available. Includes Xanax, bromazolam, clonazolam, and others. Characterized by intense potency, shorter duration, and potential antidepressant activity linked to structural overlap with tricyclic antidepressants.
Imidazobenzodiazepines — Act as partial agonists or inverse agonists at GABA-A receptors. Generally weaker and less addictive — seen as safer but less effective recreationally.
Oxazolobenzodiazepines — Prodrug-style benzos known for long durations. Some, like flutazolam, kick in quickly but convert into slow-burning metabolites (e.g., norflurazepam) that linger for 10+ hours.
Thienodiazepines & Thienotriazolodiazepines — Potent compounds featuring a sulfur-containing thiophene ring. Includes powerful designer benzos like flubrotizolam and fluclotizolam — structurally similar to TBZDs but with enhanced effects.
Thienobenzodiazepines — Rare, structurally distinct benzos with low recreational potential. Some target specific GABA receptor subunits, but few (if any) produce classic benzo effects.
Pyridodiazepines — A small group with typical benzo effects. The most notable member is lopirazepam, which retains the usual anxiolytic and sedative properties.
Pyrazolodiazepines — First described in the 1960s. Only zolazepam made it to market. Others remain obscure with minimal recreational value.
11. Pyrrolobenzodiazepines — Not psychoactive. Most are antibiotics or anti-tumor agents, such as sibiromycin or DC-81. No GABA activity.
Tetrahydroisoquinobenzodiazepines — A rare hybrid class combining benzodiazepine and isoquinoline structures. Shows promise for diverse therapeutic effects. Only one, clazolam, is of interest today.
Benzodiazepine Prodrugs — Benzodiazepine prodrugs are inactive compounds that convert into active benzos in the body, often sold as legal alternatives due to structural differences that skirt scheduling laws.
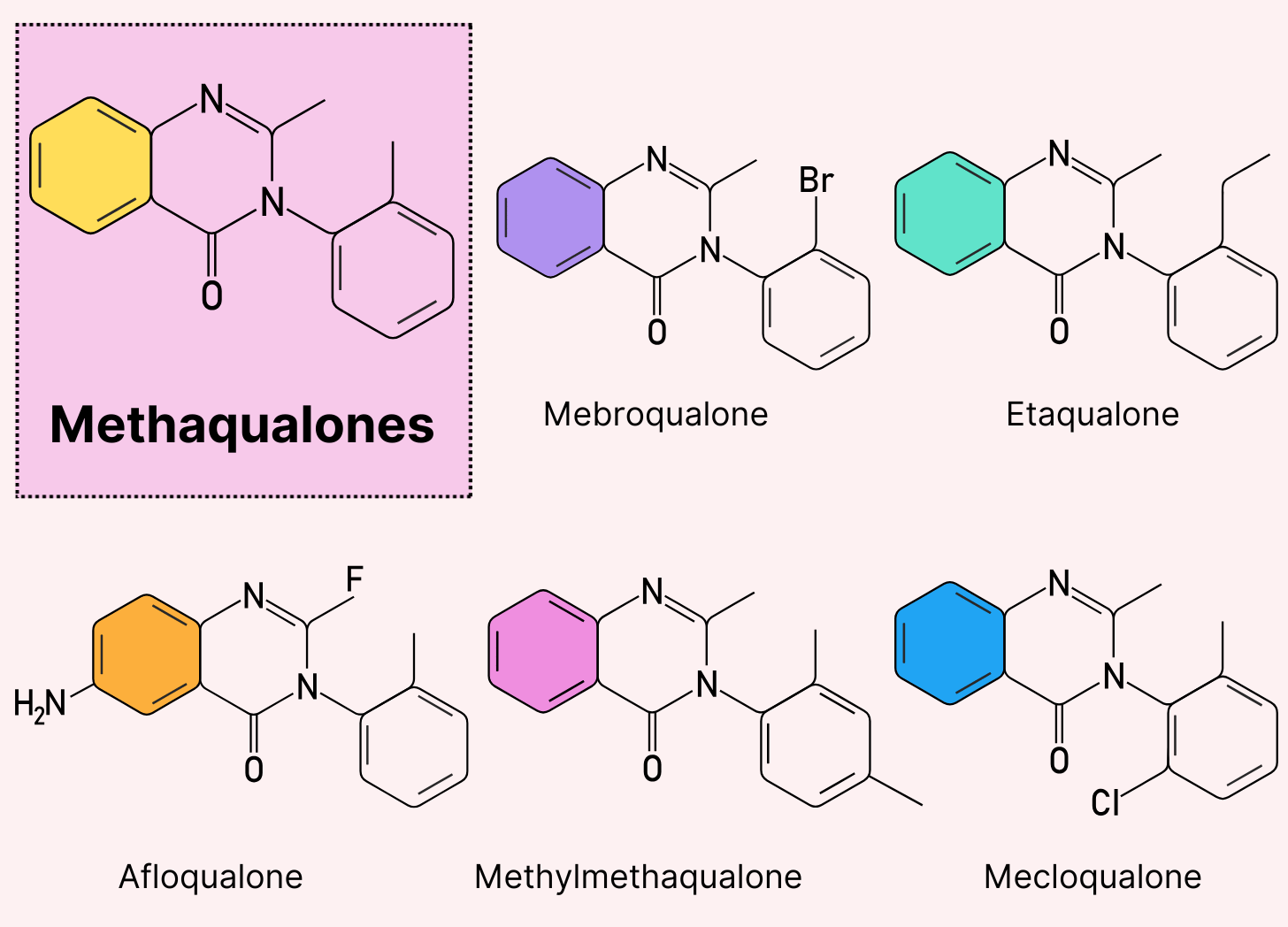
Designer Methaqualones
Methaqualone — better known by its street name “Disco Biscuits” — was a wildly popular club drug in the 1960s and ’70s. Sold under brand names like Quaalude, Sopor, and Mandrax (a combo of methaqualone and the deliriant antihistamine DPH), it was prized for its hypnotic, disinhibiting effects — similar to GHB or alcohol, but with a heavier, sedative undertone.
After a surge in recreational use, methaqualone was banned under the UN Convention on Psychotropic Substances in the late 1970s. It’s now listed as a Schedule II drug, though its medical use has vanished.
Despite the ban, methaqualone is making a quiet comeback — this time in the form of designer analogs meant to mimic the original’s effects. These include:
Afloqualone — A muscle relaxant developed in Japan with mild sedative effects and limited recreational use.
Etaqualone (ECQ) — One of the most popular modern analogs, offering GHB-like euphoria with a fast onset and short duration.
Mebroqualone (MBQ) — Closely related to methaqualone, but slightly less potent; known for a heavy body high and sleepiness.
Mecloqualone (MCQ) — Developed as a medical alternative to methaqualone, with stronger hypnotic effects and longer duration.
Methylmethaqualone (MMQ) — A potent analog often described as more stimulating than sedating, with a higher risk of side effects.
Designer Opioids
The opioids are a diverse class of compounds defined by a single pharmacological action: they bind to the body’s opioid receptors — primarily the mu-opioid receptor — to produce pain relief, sedation, and euphoria.
At the core of this group are the opiates — naturally occurring alkaloids found in the opium poppy (Papaver somniferum). These include:
Morphine — the prototypical opiate, used for severe pain relief.
Codeine — milder, often used in cough syrup and oral painkillers.
Thebaine — not used therapeutically but serves as the chemical backbone for synthesizing other opioids like oxycodone and buprenorphine.
Heroin (diamorphine) is a semi-synthetic derivative of morphine that was originally developed as a medical analgesic. However, it was moved under the Schedule I classification due to its high abuse potential.
There are now hundreds of synthetic opioids on the market — many are approved medicines — such as morphine, fentanyl, buprenorphine, hydrocodone, hydromorphone, oxycodone, and methadone. Others, like heroin and most designer opioids, are used strictly for recreational purposes or black-market distribution.
Most provide the same effects inherent to all opioids — sedation, pain relief, and euphoria.
A lot of the opioids being sold today as designer drugs were rediscovered from research done in the 1960s, when opioid development was at its peak. Several compounds have been revived from drug companies that either never made it to clinical testing or failed to gain FDA approval and were abandoned.
Fentanyl Analogs
Fentanyl is a synthetic opioid 50-100 times more potent than morphine.
Originally developed for medical use in the 1960s, it remains an important anesthetic and pain management tool.
However, its high potency makes it an attractive compound for illicit manufacturers, who have created dozens of analogs.
The designer drug market is flooded with fentanyl analogs, including:
Carfentanil — Originally developed as a tranquilizer for large animals like elephants, carfentanil is approximately 10,000 times more potent than morphine and has no legitimate human medical use.
Acetylfentanyl — About 15 times more potent than morphine, this analog has been involved in numerous fatal overdoses worldwide.
Furanylfentanyl — A fentanyl analog that, despite being less potent than fentanyl itself, has been responsible for numerous overdoses.
3-Methylfentanyl — Up to 6,000 times more potent than morphine, it appeared in the 1980s in what was called "China White."
Benzimidazole Opioids
Benzimidazole opioids are a newer, ultra-potent class of synthetic opioids — structurally distinct from both traditional opiates and fentanyl analogs.
These compounds are built around a benzimidazole ring — a nitrogen-rich structure originally explored by researchers at CIBA Pharmaceuticals in the 1950s. While some, like etonitazene, were synthesized for research, most have never seen medical use.
The danger lies in their extreme potency. Many benzimidazole opioids are hundreds to thousands of times stronger than morphine — making even microscopic miscalculations potentially fatal, especially on the unregulated street market.
Some prominent examples of benzimidazole opioids include:
Isotonitazene — Comparable in potency to fentanyl, this substance emerged around 2019 and has been linked to numerous fatalities.
Metonitazene — Slightly less potent than isotonitazene but still far stronger than morphine (between 30 and 200X more potent).
Etonitazepyne — One of the most potent opioids ever discovered, with estimates suggesting it may be several times more potent than carfentanil.
Needless to say, with the constant evolution of newer, frighteningly powerful opioids surfacing every few years, we're in for a grim future. The catastrophe brought on by the introduction of powerful fentanyl analogs to the black market has already had devastating impacts on society. The benzimidazole opioids only threaten to transform an already dire problem much, much worse.
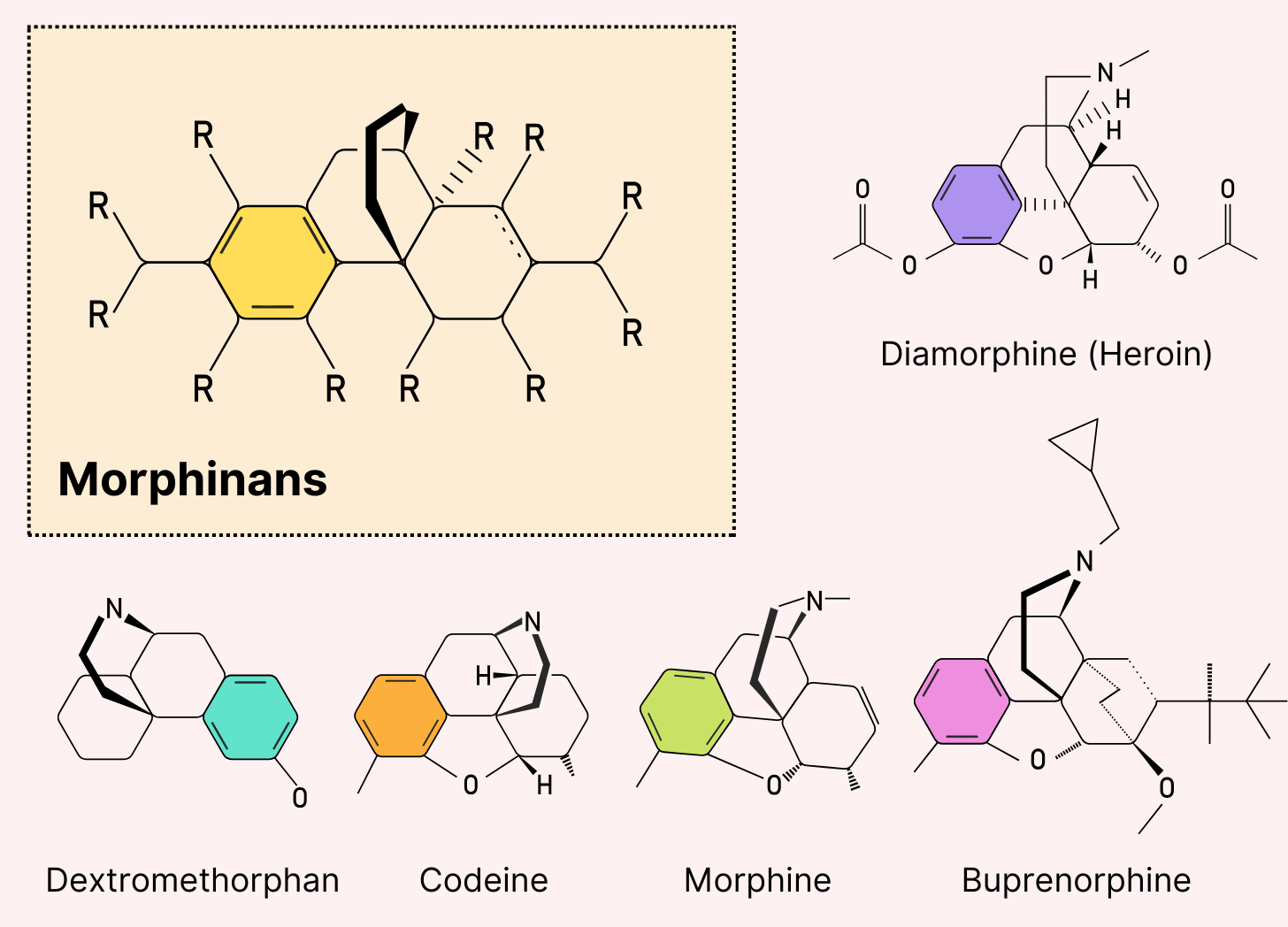
Morphinans
Morphinans are defined by a distinct four-ring chemical structure that forms the backbone of many sedative painkillers. This class includes both natural opioids like morphine and codeine (from the opium poppy), as well as semi-synthetic and synthetic drugs like hydromorphone and levorphanol.
Most morphinans exert their effects by activating mu-opioid receptors, producing pain relief, sedation, and — at higher doses — euphoria.
But not all morphinans act like typical opioids. In fact, some are better known for their dissociative effects than for pain relief. The clearest example is dextromethorphan (DXM) — a widely used cough suppressant that has little opioid activity and instead works as an NMDA receptor antagonist. (We cover DXM in more detail in our designer dissociatives article.)
Notable sedative morphinans in the designer drug market include:
3-Hydroxymorphinan — A metabolite of dextromethorphan with potential antidepressant properties.
Levomethorphan — The left-handed isomer of methorphan, which, unlike its right-handed twin (dextromethorphan), has potent opioid effects.
Butorphanol — A partial agonist/antagonist opioid used medically for pain relief.
Levorphanol — One of the most potent opioid analgesics, approximately 4-7 times more potent than morphine.
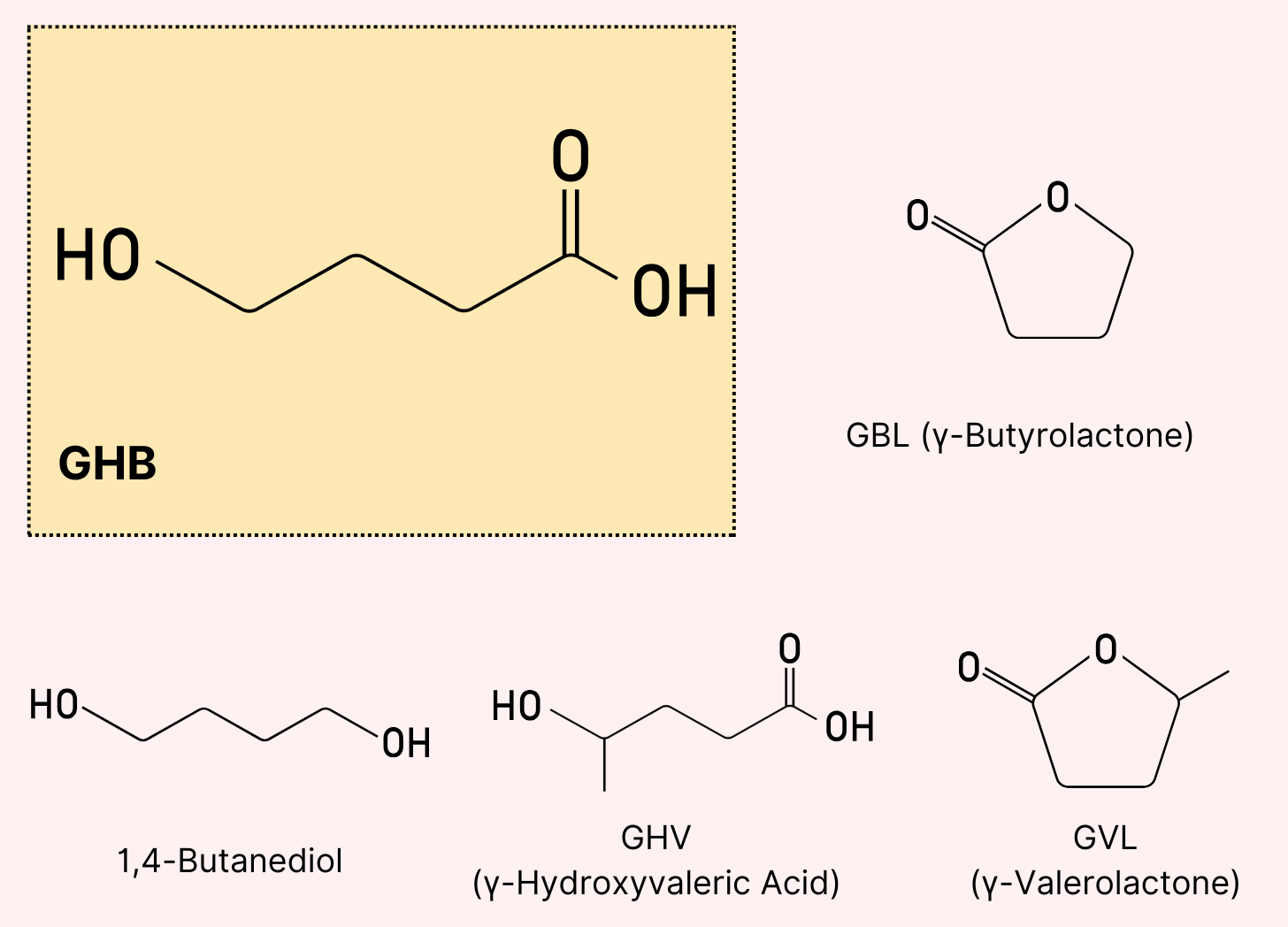
GHB Analogs
GHB (gamma-hydroxybutyrate) is a powerful central nervous system depressant — best known for its euphoric, alcohol-like effects. Odorless, colorless, and active in tiny doses, it’s easy to conceal and notoriously difficult to dose safely.
Before its ban in 1990, GHB was marketed in health stores as a performance enhancer. Today, it remains a popular underground party drug — especially at festivals — thanks to its low cost, strong euphoria, and similarity to alcohol or MDMA.
Its potency, invisibility, and rapid onset also make it a frequent tool for covert use or abuse, raising major concerns around safety and consent.
There are four main GHB analogs available today as designer drugs; all have very similar effects:
GBL (γ-Butyrolactone) — This is a prodrug of GHB, which means that once consumed, the liver converts it into the active form. GBL is often used industrially as a solvent, making it easier to obtain than GHB in some regions.
1,4-Butanediol — Another prodrug of GHB that converts to GHB in the body. It's commonly used in the production of plastics, making it relatively accessible.
GHV (γ-Hydroxyvaleric Acid) — A GHB analog with slightly weaker effects and a longer duration of action.
GVL (γ-Valerolactone) — The lactone form of GHV, similar to how GBL relates to GHB. Like GBL, it's converted to its active form (GHV) in the body.
The high potency of GHB and its analogs is a double-edged sword. While users only need a small amount to feel the effects (thus ensuring it stays relatively cheap), it's very easy to take too much, which not only renders the user completely unconscious but can also be fatal.
The line between an enjoyable dose and an overdose can be dangerously thin with these substances.
Volatile Anesthetics
Volatile anesthetics are a class of inhalational compounds that evaporate easily at room temperature and produce rapid sedation and unconsciousness when inhaled.
Diethyl ether is both the oldest and most famous within this group. It was one of the first anesthetics used in surgery, dating back to the 1840s.
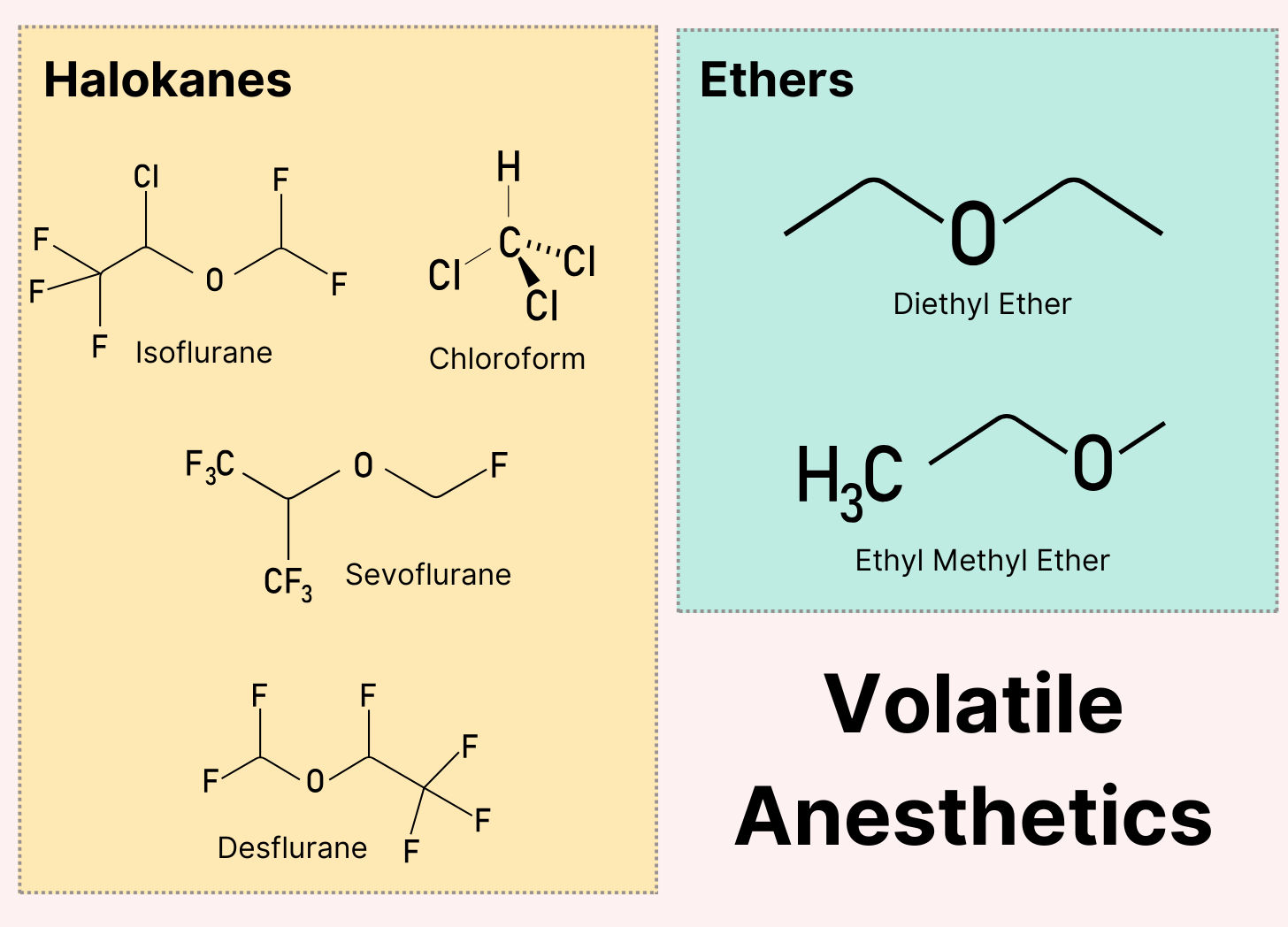
Other volatile anesthetics include the haloalkanes isoflurane, sevoflurane, chloroform, and desflurane. These compounds contain halogen atoms (like fluorine or chlorine) attached to carbon chains. Diethyl ether is technically classified as an ether (containing an oxygen atom between carbon atoms), but the effects are virtually identical.
The volatile anesthetic class works by hijacking both the GABA and NMDA systems to create euphoria, disinhibition, and dissociation similar to alcohol intoxication — but with a more dreamlike quality.
The high volatility of these compounds makes them particularly dangerous to handle — the vapors are flammable, explosive, and can cause rapid unconsciousness when inhaled in concentrated form.
Sedative Hypnotics Are The Dark Mirror of the Psychedelic Renaissance
In an era where psychedelics are used to confront trauma and expand consciousness, the rise of sedative hypnotics and synthetic opioids reveals a darker trend — one rooted in the desire to feel nothing at all.
Where one path seeks meaning, the other seeks escape.
This isn’t just a crisis of chemistry — it’s a crisis of consciousness.
Designer Drug Series
This has been part 6 in a 10-part series on designer drugs.
Read some of our past series using the links below, or subscribe to receive new posts as they’re released:
Part 8: Sedative Hypnotics & Opioids
Part 9: Deliriants (Subscribe)
Part 10: Atypical Designer Drugs (Subscribe)
Help Us Grow 🌱
Tripsitter was built by a community of psychedelic advocates — but it’s people like you that allow us to thrive.
You can also follow us on Bluesky or subscribe to our Reddit.









This is great information!