Trip Killers: Hitting the Psychedelic Emergency Brake
Trip killers can end a bad trip in minutes — but they carry risks that make them a last resort, not a shortcut.
Sometimes, psychedelics show us exactly what we need to see. Other times, they drag us into a nightmare we’d give anything to escape.
When fear takes over, the instinct is to fight, but often the safest way through is to let go and allow the mind to move where it’s resisting.
Still, there are rare situations where a trip becomes dangerous — to the person or those around them. In these moments, medical professionals and trained sitters may use “trip killers” to put a rapid end the psychedelic experience.
Trip killers are not tools for casual use — they’re prescription medications with serious risks that should only ever be administered by qualified professionals.
Not only can these drugs be dangerous, but the hard truth is that many difficult trips carry their own medicine — stopping them too quickly can interrupt the very process that makes psychedelics transformative.
What Are Trip Killers?
Trip killers (sometimes called hallucinogen antidotes) are substances that can take the edge off — or even shut down — a psychedelic trip. Think of them as the emergency exit when things go from challenging to completely unmanageable.
They’re not magic buttons, though. Different psychedelics respond to different trip killers, and sometimes nothing will work at all.
These aren’t casual tools. Trip killers are strong, often risky drugs — and the dose matters just as much as the choice of substance. Used the wrong way, they can cause more harm than good.
That’s why they should only ever be a last resort — ideally in the hands of a doctor or trained guide. Still, when a trip crosses the line into real danger, they can do what they’re meant to: stop the trip and bring you back to reality as quickly as possible.
Top 7 Trip Killers
The go-to trip killers are benzodiazepines — fast-acting, reliable, and effective at shutting down a trip. They’re the closest thing to an “off switch” most people know.
But benzos come with serious risks: they’re addictive, dangerous when mixed with other depressants, and not suitable for everyone. For those who can’t (or shouldn’t) use them, there are alternatives like certain sleep aids and antipsychotics.
When benzos aren’t an option, certain antipsychotic medications can serve a similar role. These work differently in the brain but can be just as effective at dulling psychedelic effects — especially tryptamines like LSD, psilocybin, or DMT.
There’s also a separate tool worth noting called activated charcoal. This all-natural health supplement doesn’t “kill” a trip once it’s underway, but if taken immediately after ingesting certain types of drugs, it can bind to the compound in the stomach and prevent any more from being absorbed. Doctors sometimes use it in emergency rooms for overdoses, but timing is everything — once the substance is in the bloodstream, charcoal won’t help.
Here’s how the most common options compare, from fast-acting benzos to slower antipsychotics.
1. Alprazolam (Xanax)
The fastest benzo for killing a trip. Kicks in within 15–45 minutes and lasts 4–6 hours. Quick relief, but often wipes your memory of the night. Expect heavy drowsiness, and be careful — mix it with alcohol or other downers and blackouts are almost guaranteed.
2. Lorazepam (Ativan)
A slower start than Xanax (20–45 minutes), but sticks around for about 8 hours. Great for longer psychedelics like DOX or 2C-X. Usually knocks you out cold, which can be a blessing after a rough ride.
3. Diazepam (Valium)
Takes its time — up to 2 hours unless chewed — but lasts over 12 hours once it hits. Smooths out looping thoughts without totally erasing the trip. Less of a “sledgehammer” than Xanax or Ativan, more of a steady calm.
4. Clonazepam (Klonopin)
Slowest of the bunch (1–4 hours to peak), but it lingers — half-life is around 40 hours. Not the most popular because of the delay, though some like its subtle euphoria. Handy if nothing else is available.
5. Zolpidem (Ambien)
Technically a Z-drug, but acts a lot like a benzo. It works — but usually by knocking you out completely. Memory gaps are common. A bit safer than benzos in some ways, but still risky with alcohol or other depressants.
6. Quetiapine (Seroquel)
An atypical antipsychotic. Takes 20–60 minutes to kick in. Often used when benzos aren’t an option. It dulls the trip but comes with heavy sedation — you’ll probably be out for the night.
7. Olanzapine (Zyprexa)
Another antipsychotic, especially good for classic psychedelics like LSD, psilocybin, and DMT. Not as effective for things like MDMA or ketamine. Starts working in about 30 minutes and lasts several hours.
How Do Trip Killers Work?
Not all trip killers work the same way — some calm the mind, others block the psychedelic at its source.
Benzodiazepines — like Xanax, Valium, and Ativan — act by turning up the volume on a neurotransmitter called GABA, which functions as the brain’s natural brake pedal.
When GABA activity rises, mental chatter slows, anxiety eases, and the body shifts into a calmer state.
At lower doses, this doesn’t fully erase the psychedelic, but it takes the edge off — the panic and racing thoughts fade into the background, even if the visuals remain.
At higher doses, the sedation can be so strong that you simply fall asleep, which in practice ends the trip. This is why benzos are a first-line option in medical settings: they don’t always kill the psychedelic outright, but they make the situation safe by calming the storm.
Antipsychotics — like Seroquel and Zyprexa — take a different route. Instead of pressing the brakes, they block the actual receptors psychedelics need to work. The main target here is the 5-HT2A serotonin receptor, which is where most classical psychedelics (think LSD, psilocybin, and DMT) latch on to induce their hallucinogenic effects. By occupying these receptors, antipsychotics interrupt the psychedelic “signal,” cutting the intensity of the trip or shutting it off altogether.
How Long Do Trip Killers Take To Kick In?
Every trip killer has its own timeline. Some calm things down in minutes, others take an hour or more.
These times refer to oral use — swallowing or chewing for faster absorption.
NOTE: It’s not safe to smoke, inject, or snort these drugs.
Alprazolam (Xanax): 10–20 minutes
Lorazepam (Ativan): 20–45 minutes
Clonazepam (Klonopin): 45–60 minutes (peak may take 1–4 hours)
Diazepam (Valium): 1–2 hours (faster if chewed)
Zolpidem (Ambien): 15–30 minutes
Quetiapine (Seroquel): 20–60 minutes
Olanzapine (Zyprexa): ~30 minutes
Activated Charcoal: Immediate if taken right after ingestion
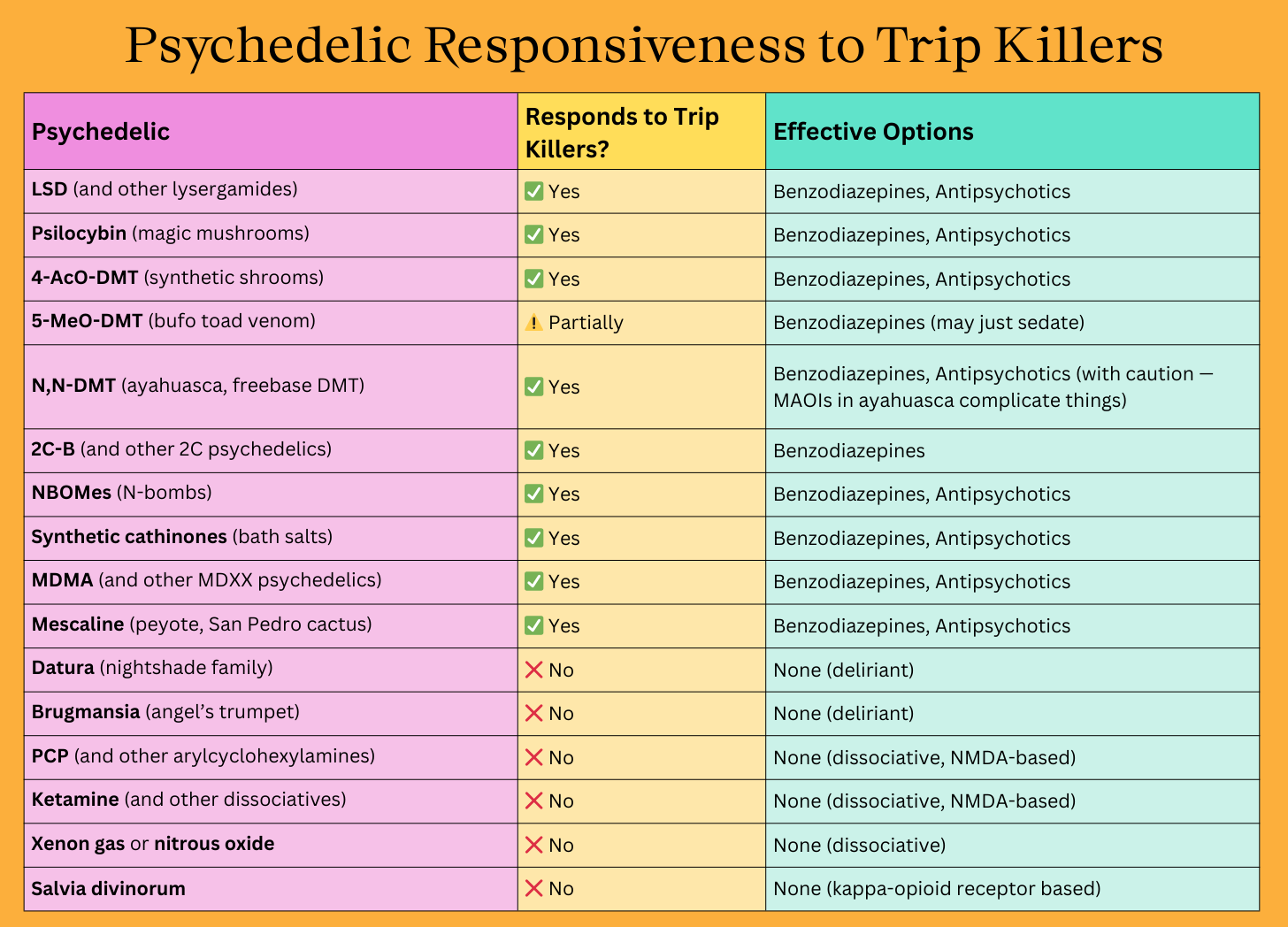
Which Psychedelics Respond to Trip Killers (and Which Don’t)
Trip killers aren’t universal. Benzos and antipsychotics can calm or stop many classic psychedelics — like LSD, psilocybin, and DMT — because those drugs rely heavily on serotonin receptors. But not every psychedelic plays by the same rules.
Dissociatives like ketamine or PCP act on NMDA receptors, not serotonin, so benzos and antipsychotics won’t “switch them off.” In fact, combining sedatives with dissociatives can actually increase risk. The same goes for plants like salvia or datura — their chemistry is so different that there’s no reliable way to kill the trip once it starts.
The takeaway: not every psychedelic has an off switch. If you’re exploring a substance, it’s crucial to know in advance how it works, how long it lasts, and whether a trip killer would even make a difference.
Alternatives to Trip Killers: Riding Out a Difficult Trip
Most difficult trips can be transformed with patience, support, and surrender — trip killers should only enter the picture when safety is truly at risk.
Here are some non-pharmaceutical tools that can make a difficult trip safer and more manageable:
For the person tripping:
Breathe and ground yourself — Slow, rhythmic breathing goes a LONG way. Feeling your feet on the floor or holding something or someone familiar can also help anchor you.
Change the setting — Move to a quieter or more comfortable space, lower the lights, or put on calming music.
Hydrate and rest — Sipping water and lying down in a safe spot can ease overstimulation.
Let go of resistance — Many bad trips intensify when you fight the experience. Surrendering often makes it easier to move through.
Trust your sitter — If you have someone watching over you, lean on them for reassurance. Sometimes just hearing “you’re safe” is enough.
For trip sitters:
Stay calm and present — Your steady energy can help anchor someone who's struggling to ground themselves.
Reassure and normalize — Remind them that the effects are temporary and they will come down sooner or later.
Reduce stimulation — Turn down lights, sounds, and distractions. Red spectrum lighting helps.
Offer gentle grounding — A blanket, a hand to hold, some water, or calm breathing together.
Watch for danger signs — If they’re having seizures, trouble breathing, chest pain, overheating, showing signs of psychosis (violent or delusional), or are unresponsive, this is no longer just a “bad trip.” Call emergency services immediately.
More Resources About Difficult Psychedelic Experiences
Psychedelic Safeguards with Jules Evans (Podcast)
Grow Your Own Mushrooms at Home
SporesMD is offering Tripsitter readers 20% off all spores.
Use TRIPSITTER at checkout.
Enjoying Tripsitter? 🍄
Don’t Journey Alone! Tripsitter was built by a community of psychedelic advocates — but it’s people like you that allow us to thrive.
You can also follow us on Bluesky or subscribe to our Reddit.